Obamacare Website Fails as Deadline Arrives
BY MAGGIE FOX, NBC News
People trying to apply and enroll for private health insurance through Obamacare before Monday's midnight deadline discovered the website was "currently unavailable."
Healthcare.gov, the online marketplace bedeviled by bugs since its launch last fall, went down for several hours Monday morning, a statement from the Department of Health and Human Services said. It was back online later in the morning after a short time when it put customers in a "queue," meaning they'd be notified by email when they could proceed with enrollment...
Should be an interesting day for "KatrinaCare."
The day's other main event is the pending Senate vote to kick the SGR and ICD-10 cans down the road yet again, this time past the 2014 mid-term elections. I'll be following that today.
__
athenahealth Issues Statement on ICD-10 Delay; Government's Willingness to Kick the Can Down the Road on SGR, Meaningful UseMEANWHILE
WATERTOWN, Mar 31, 2014 (Menafn - GLOBE NEWSWIRE via COMTEX) --athenahealth, Inc.ATHN, a leading provider of cloud-based services for electronic health record (EHR), practice management, and care coordination, today issued the following statement in reaction to the House vote, and pending vote from the Senate, to patch the Sustainable Growth Rate ("SGR" or "Doc Fix") and delay ICD-10 for another year to October 2015.
Ed Park, executive vice president and chief operating officer, athenahealth, provided the following comment:
"It is unfortunate that the government has once again chosen to delay ICD-10. athenahealth and its clients are/were prepared for the ICD-10 transition, and in fact we have national payer data showing that 78 percent of payers are currently proving readiness in line with the 2014 deadline. The moving goal line is a significant distraction to providers and inappropriately invokes massive additional investments of time and money for all. The issue is even more serious when considered in association with another short-term SGR fix and 2013's Meaningful Use Stage 2 delay. It is alarmingly clear that health care is operating in an environment where there is no penalty for not being able to keep pace with necessary steps and deadlines to move health care forward. Our system is already woefully behind in embracing technology to drive information quality, data exchange, and efficiency, and delays like this only hinder us further."
Why Doctors Are Not Joining ACO’s
March 31, 2014 10:09 am by Dr. Linda Girgis, MD
According to a recent study published on Wiley Online Library, 60% of physician practices have not joined and have no intention of joining an ACO in the future ... Of the 32 medicare pioneer ACO’s : 9 dropped out, 13 had “some” savings, and 2 lost money and had to pay CMS. The ones that had “some” savings did not necessarily have enough to get paid ...Full MedCityNews article here.
There are many reasons that doctors are not rushing to join ACO’s”
1. As noted above, this is a new venture and may very well fail. There is no record to study to make a wise investment.
2. We are only allowed to join one. We are not allowed to change once we sign up. What if we choose the wrong one?
3. It is another intrusion into the way we practice. We are now required to meet increasing government regulations, ie meaningful use, e-prescribing, etc. This is another way for insurers to regulate the way we practice.
4. We can lose money. Most doctors are truly trying to give the best care for our patients. We try to be cost conscious about it. We are the ones on the front lines who know the patient best and can make the best treatment decisions. We do not need an organization to hold us accountable for costs. Some patients are truly sick and require expensive diagnostic work up. I don’t want to have it in the back of my mind that I may get “dinged” for ordering an expensive test that I think a patient needs. For doctors, quality comes first. Sure, we all need to take some responsibility for holding down costs, but I fear the day when we are punished for doing the best for our patients.
5. Most ACO’s are not physician run. The quality measures are being made by non-physicians. Quality metrics can only be determined by someone who has a medical degree. If others are determining what makes up good outcomes, they are basing their decisions on statistics and not medicine. Clearly, a deficiency in my mind.
6 The future is uncertain. With the passage of the ACA, many physicians are concerned about the future of the healthcare system in this country. Many fear the worst. Many are in a “wait and see” position before making any decisions about changing the way they practice.
7. Doctors have been burned by insurance companies and regulations in the past. Most are not trusting the new ACOs based on past experiences...
__
MEANINGFUL USE STAGE 2:
INTERVIEW WITH RANDY HOUNTZ, INDIANA REC
How prepared are providers in Indiana for Stage 2 Meaningful Use?Good stuff. Props to EHR Intelligence.
It’s been fascinating to watch Stage 2 unroll as compared to Stage 1. We’re in the same spot where people glance at a lot of the requirements and metrics and think, “That’s not that hard especially after I’ve done Stage 1. This is just a few new things; it’s not going to be that difficult.”
Just as we saw in Stage 1 when people started to dig into the details, they are realizing that it may be a little bit more complicated than what they had anticipated. It’s not surprising but Indiana folks in Indiana are starting to realize that Stage 2 is hard and they’re going to need some help to get there. Obviously, we’re in a good position to do that.
What factors will determine whether an eligible provider is successful or unsuccessful in Stage 2?
The challenge is going to be different based on the size of the organization. In Indiana, we have a significant amount of provider employment, employed by hospital systems specifically, and they have to look at global solutions for transitions of care. They can’t look at one doctor out of 475 doctors — one a provider to provider basis — and just his transitions of care and how to they get to 10 percent. They have to be thinking of some global solutions for that. We are very fortunate to have a very good HIE in the state that has a global solution and for them now it’s a matter of getting in queue. It’s bandwidth from an HIE standpoint for them to get all aligned and integrated.
For a small provider it’s much more difficult because they probably can’t buy that solution. They’re going to have to do a little more of that detailed work of whom am I referring out to and then they’re going to have to do some more work to determine if those providers are on Stage 2 software or a piece of a HISP somewhere because if they’re not this HISP to HISP thing doesn’t work. That’s the biggest challenge I see for small providers — that physician they are referring to has to also be on a HISP to get that transition of care piece to work.
Is the Purdue REC in communication with these HIEs in order to help providers?
Absolutely, we talk to them if not every week then every other week. Our main HIE in the state also does work with syndromic surveillance messaging to the state’s Department of Health as well as immunizations. We’re fortunate in the state to have several HIEs, and we keep open communications with all of them. The whole transitions of care — that has really just started to crystallize in the last two months as far as what is a real process that can happen to make it work. We’ve been talking about hypothetical HISPs, HIEs, and eHealth partners. Now it’s shifted to workable plans.
Is integrating HIE into clinical workflows going to pose a problem?
It is. For large providers, they’re probably going to make that workflow fairly straightforward for providers or their staff. It’s going to be a concern for small providers and it’s going to depend on the software. On top of that, they’re going to have to configure their software to set up where that referral is going and what their Direct address is and their EHRs need to verify their security key and all those technical components. It’s really going to be tough.
__
ERRATUM: HAT TIP TO THE INCIDENTAL ECONOMIST
__
KICK-THE-CANS CODA
Medscape Medical NewsDon't hold your breath for a "signing ceremony."
Senate Votes to Delay SGR, ICD-10 by 1 Year
Mark Crane, March 31, 2014
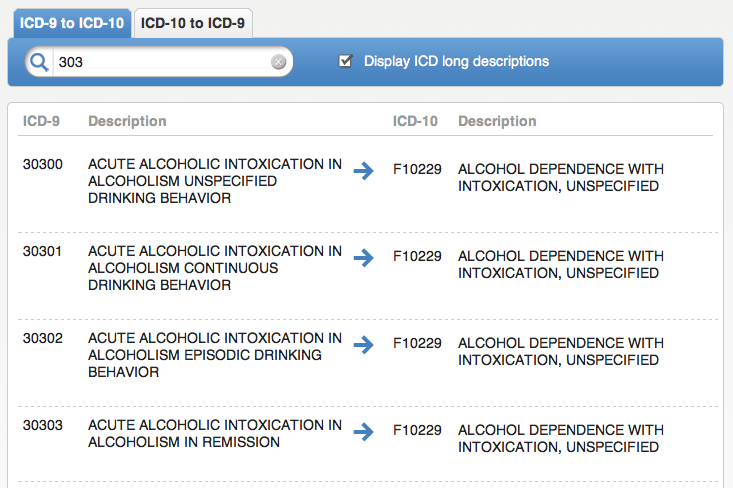
The US Senate has voted for a 1-year "doc fix" preventing a 24% pay cut for physicians who treat Medicare patients, while also delaying by 1 year the implementation of the nationwide conversion to the International Classification of Diseases, 10th Revision (ICD-10), set of diagnostic and procedural codes that was scheduled to occur on October 1.
The bill now awaits President Obama's signature...
___
More to come...