Apologies for the mixed metaphor (do trains have odometers?). Six months and seven days. That time will evaporate quickly.
I now subscribe to Health Affairs. Recent paper excerpt below.
WHAT'S THE ISSUE?From Medcity News:
On October 1, 2014, all health plans, health data clearinghouses, and health care providers that transmit health information electronically must use a new, significantly broader, coding system, called ICD-10, for diagnoses and inpatient procedures. The new system has the potential of improving the health care system, but its costs and complications have caused some to question whether the costs outweigh the benefits.
WHAT'S THE BACKGROUND?
ICD is the acronym for the International Classification of Diseases. The ICD is maintained by the World Health Organization (WHO) to classify diseases and other health problems recorded on many types of health and vital records such as death certificates. It is used to monitor the incidence and prevalence of diseases and other health problems. The ICD is periodically revised to incorporate changes in the practice of medicine. In 1990 WHO adopted the 10th revision (ICD-10).
In the United States, ICD-10 has been used since 1999 to code and classify mortality data from death certificates. However, a modification of the 9th revision (ICD-9) is still used to assign codes to diagnoses associated with inpatient, outpatient, and physician office use and for inpatient procedures. Currently, the United States is the only G7 nation (the other G7 nations are Canada, France, Germany, Great Britain, Italy, and Japan) continuing to use ICD-9...
WHAT'S IN THE LAW?
...In January 2009 HHS published final regulations calling for a transition to ICD-10 and set October 1, 2013 as the compliance date. However, in late 2011 and early 2012 three is- sues emerged that led the secretary to reconsider the compliance date for ICD-10: 1) The industry transition to the version 5010 electronic operating system necessary to accommodate ICD-10 did not proceed as effectively as expected; 2) providers expressed concerns that other statutory initiatives were stretching their resources; and 3) surveys and polls of affected parties revealed a lack of readiness for the ICD-10 transition. As a result, in August 2012, HHS announced a delay of the implementation date for ICD-10 to October 1, 2014. This means that ICD-10 codes must be used for services provided on or after October 1, 2014. ICD-9 codes may only be used for services provided before that date.
WHAT'S THE DEBATE?
Conversion from ICD-9 to ICD-10 is complicated and costly, causing some affected parties to question whether the benefits of the con- version outweigh the costs. Experts say the new code set will have an impact on not only claims submissions but also such processes as patient eligibility verification, preauthorization for services, documentation of patient visits, research activities, and public health and quality reporting. Not only must new software be installed and tested, but training for physicians, staff members, and administrators is required. New practice policies and guidelines must be developed, and paperwork and forms updated.
Proponents of the transition to ICD-10, including the federal agencies that developed the system, say the codes will provide a more exact and up-to-date accounting of diagnoses and hospital inpatient procedures, which could improve payment strategies and care guidelines. Codes describing the circumstances of injuries are important for public health researchers to track how people get hurt and try to prevent injuries...
Opposition to implementation of the ICD-10 transition in 2014 comes primarily from medical associations, including the American Medical Association (AMA). They believe that the transition will be overly burdensome on providers who are already engaged in efforts to comply with new systems and requirements such as meaningful use, e-prescribing, and quality data reporting.
They cite costs as a major problem. Estimates regarding the additional costs of the implementation of ICD-10 have varied, but one study in 2008 sponsored by the AMA, the Medical Group Management Association, and other provider associations has pegged the adoption costs for a small practice at $83,000, ranging up to $2.7 million for a typical large practice. The study identified costs in six key areas: staff education and training, business process analysis, new claims form software, IT system changes, increased documentation costs, and cash flow disruption...
WHAT'S NEXT?
Given the political fallout from the data system problems encountered with implementation of the health insurance exchanges, the Obama administration will likely be extremely sensitive to any potential problems with claims processing due to the ICD-10 conversion. Extensive testing, both of the system’s connectivity and of coding accuracy, is needed to ascertain readiness for the conversion. As the implementation date approaches, CMS will have to decide if there has been sufficient progress to keep to the deadline. Since CMS has concluded that concurrent use of both ICD-9 and ICD-10 (at user discretion) would be overly complicated, confusing, and costly, likely action in case of significant unreadiness would be to again delay the implementation date.
Where Doctors Should Be In The Onward March Of ICD-10Item number 5: REC opportunity?
March 25, 2014 by Dr. Linda Girgis, MD
There is much fear and concern among doctors and other healthcare workers surrounding the implementation of ICD-10. Many are predicting a delay in reimbursements in October when ICD-10 is made mandatory for insurance reimbursement. Surely those who wait to near the deadline will have problems. Doctors should be preparing from now, if not sooner.
Where Should Doctors Be in the ICD-10 Conversion?
- All doctors should know coding. Ultimately, we are the ones responsible for any billing or coding mistakes. We cannot pass the blame on someone else. The buck stops at us. The best way to protect ourselves from coding and billing mistakes is to be proficient in it. While many rely on others for this task, we still need basic knowledge and oversight of our billing practices, despite who is actually doing the coding.
- Doctors should be learning ICD-10 coding. There are many seminars, webinars, on-line materials and many sources available to teach us. We need to start utilizing some of these references now. If we wait to September to start, we will be learning in crunch time and this is the way mistakes seep in. Better learn from now when we have the leisure to make and learn from mistakes.
- Doctors and practices should have already or currently be mapping their codes. What this means is that the most commonly used codes should be mapped out into their ICD-10 equivalents. It will no longer be acceptable to just code for knee pain. Now, the code needs to show the cause and exact location. What could have been only coded with only one ICD-9 code in the past, now has many more detailed ICD-10 codes to choose from.
- Some insurances are allowing codes to me submitted in the ICD-10 format from next month. What I am planning to do in my practice is to make a trial run with one insurance at a time. In this way, I will not have a major delay in reimbursements and I have time to work out any flaws in the implementation process. This also gives me a more ample way to become proficient in ICD-10 coding.
- We need to ask for help. There are many people available to help. Many of our state and national medical societies have help available for us. We need to search out these resources and use them...
__
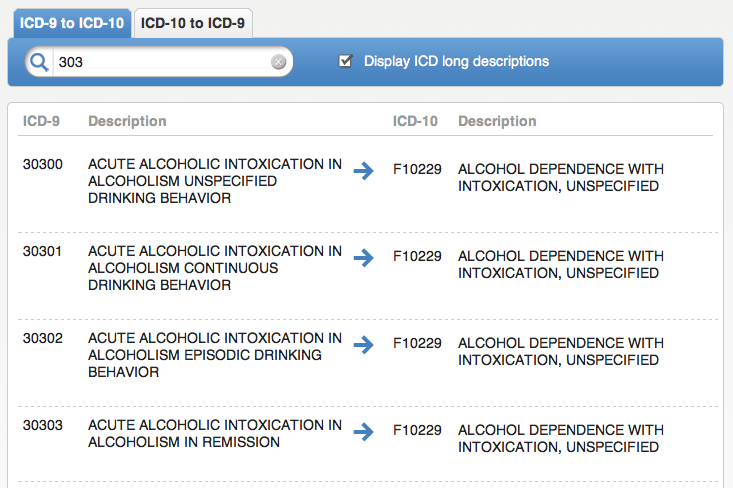
One thing a lot of people are unaware of is that the ICD-9 to ICD-10 crosswalk mapping is not unilateral. There are some ICD-10 codes for which there is no ICD-9 antecedent, and, in some cases the ICD-10 code is less granular than the ICD-9.
From the AMA guidance:
A critical issue associated with the transition to ICD-10 involves the matter of crosswalking between the ICD-9 and ICD-10 code sets. The term “crosswalking” is generally defined as the act of mapping or translating a code in one code set to a code or codes in another code set. (The terms “crosswalking” and “mapping” are sometimes used interchangeably.) There has been much discussion about how crosswalks will be used in the industry during the transition from ICD-9 to ICD-10. Understanding crosswalking will be important to physicians during the transition phase when learning which new ICD-10 code to use in place of an ICD-9 code, since there is not always a one to one match.
Were the crosswalk unidirectional, you can envision an EHR drop-down menu subpanel wherein you'd simply pick the more granular ICD-10 code from your former usual ICD-9 code choice. A few seconds more** per chart, perhaps.
** Even so, assume an average additional 3 seconds per chart, processing 5,000 patient visits per year, 15,000 seconds, or 4.16 hours, at $240 per hour (see my "Case for EHR scribes?" post), that's an additional $1,000 annual labor cost. Then there would also be the inevitable rejected claims re-processing costs, at least in the early going.Not gonna be that simple. 1.2% of ICD-10s have no ICD-9 antecedent. 3% of ICD-9s have no ICD-10 match at all.
Below, an example of reduced ICD-9-to-10 granuarity.
__
About that mixed metaphor. :)
__
THCB UPDATE
The Note Taker's Dilemma
Saurabh Jha, MD
The year is 2020, or sometime in the future when the healthcare system is better, much better. Patients have access to their medical notes, are encouraged to read the notes regularly and ask physicians relevant questions. This is to facilitate patient-centered participatory medicine (PCPM), previously known as shared decision making. In fact, note reading by patients is now a quality metric for CMS.
The CEO of the Cheesecake Hospital Conglomeration, one of the hospital oligopolies, has set up a Bureau for Transparency and Protection of Patients from Complex Medical Terminology. The goal is to risk manage troublesome medical writing that could result in poor satisfaction scores, complaint or a lawsuit.
Mr. Upright (MU) is the Inquisitor General for the bureau. He has called the author (SJ), a repeat offender, to his office to discuss elements of his medical record keeping...
Read on.
___
More to come...





No comments:
Post a Comment